Confounding Social Determinants
There is poverty in America. There always has been. There probably always will be. It is unfortunate and we must always strive to make a difference in the lives of those who are not as fortunate as most Americans. Poverty cuts across all races, ethnicities, sexes, geographies and whatever other labels we like to use. It is a human problem. Another human problem we experience in the US (and pretty well all countries) is healthcare. Too often there are good intentions that really are just confounding social determinants and slowing progress to transform our “sick care” system to a real healthcare system.
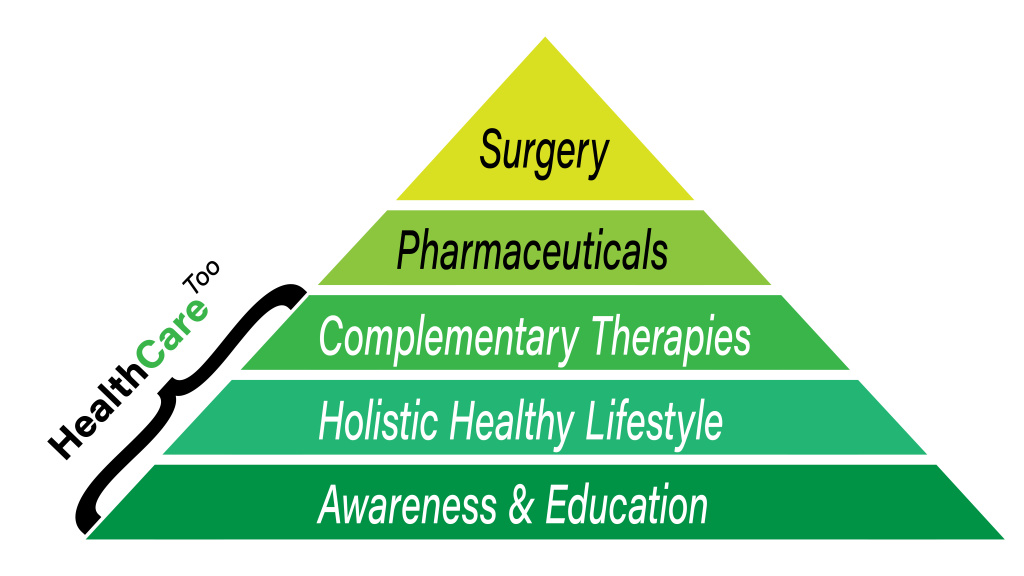
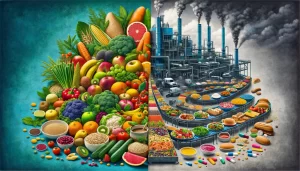
Social determinants of health are those non-clinical factors that bear greatly on health like education, nutrition, transportation, and genetics. Nothing about pills or procedures. For most people social determinants are 80% or more of what determines health, whether rich or poor. Despite Congressman Cassidy’s quote in the article, prosperity is not the key to health outcomes. Healthy lifestyles are the key to health outcomes. The US spends approximately 80% of its healthcare dollars annually to treat (not cure) chronic diseases that are rooted in lifestyle decisions. Our health system is good at disease management, not prevention and not cures. Until we stop confounding social determinants with social justice issues, we will continue to waste dollars and lives… rich, poor, black, white, Asian, American Indian, Appalachian, all those we want to help. We are all human. No one wants to be sick. Everyone benefits from proper nutrition, moderate exercise, loving relationships and positive social interactions. The best way to help low-income communities is to help all Americans… provide real healthcare for everyone and not disease management for a few.
Integrating SDH interventions into healthcare delivery is likely to nudge some individual health outcomes. However, recent and pervasive discussions about SDH suggest a belief among many that they are the Holy Grail for achieving the long-sought but elusive health outcomes for low-income populations. These discussions with study participants suggest a need to further evaluate proposed approaches for and expectations from burgeoning SDH interventions. Achieving population-based shifts in health outcomes for low-income communities requires moving far beyond text message reminders, Uber rides to clinic visits and vouchers for farmer’s markets and food pantries. These shifts demand bold and transformative steps to address poverty by providing education, economic opportunity and a pathway to lifelong economic stability. Congressman Bill Cassidy also said, “Prosperity is the key to improving health outcomes”. As we develop interventions for the social determinants of health, unless we begin to heed this message, in the years ahead rather than finding the Holy Grail, we will instead certainly find ourselves on the path to a dead-end road.
Source: Social Determinants Of Health: Holy Grail Or Dead-End Road?
You might also enjoy these articles:
Social Determinants Of Health: Another Healthcare Fad?
‘Toxic stress’ on children can harm their lifelong learning, mental and physical health